Deferring antiviral therapy for hepatitis C until a person progresses to advanced liver disease has clear drawbacks including lower treatment effectiveness and an increased risk of clinical events and death, according to a study of US veterans presented at the European Association for the Study of the Liver (EASL) 50th International Liver Congress last month, in Vienna, Austria.
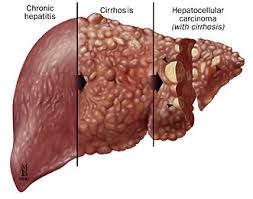
Over years or decades, chronic hepatitis C virus (HCV) infection can lead to serious liver disease including cirrhosis, hepatocellular carcinoma (liver cancer) and need for a liver transplant. When the standard of care for hepatitis C was interferon-based therapy – with its long course of treatment, poor tolerability and only modest cure rate – experts generally recommended delaying treatment until a patient developed advanced disease.
Now that much more effective and well-tolerated interferon-free direct-acting antiviral therapy is available, a growing number of providers and advocates think everyone living with hepatitis C should be eligible for treatment. But treatment is still often limited to the sickest patients due to the high cost of the new drugs.
Jeffrey McCombs, a health economist at the Schaeffer Center for Health Policy and Economics in Los Angeles, and colleagues, compared treatment outcomes for people with hepatitis C treated before or after development of advanced liver disease.
Read the full article here: AIDSMAP