Rates of gonorrhea, a sexually transmitted disease, are rising sharply in California, especially among gay and bisexual men, according to new state health data.
The gonorrhea rate among California men aged 15 to 44 shot up 54 percent between 2011 and 2014, according to recently released data from the California Department of Public Health. Among women in the same age group, it rose 35 percent.
An average of 34,000 gonorrhea cases among 15-to-44 year-olds was reported in California each year between 2012 and 2014, most of them among men.
By contrast, the national gonorrhea rate, calculated slightly differently than California’s, rose about 15 percent among men aged 15-44 between 2010 and 2013, the latest available data for that group.
Public health experts say the reasons for gonorrhea’s resurgence in California are complex. It may reflect better screening, which detects cases that would not have been found previously.
Other possible explanations include lower condom use among young people and the rise of Tinder and other “hookup” apps that promote multiple sex partners. But experts say there’s not enough data to pin the rising gonorrhea rates on any one cause.
Clinicians say they are frustrated they haven’t made more headway in controlling the disease.

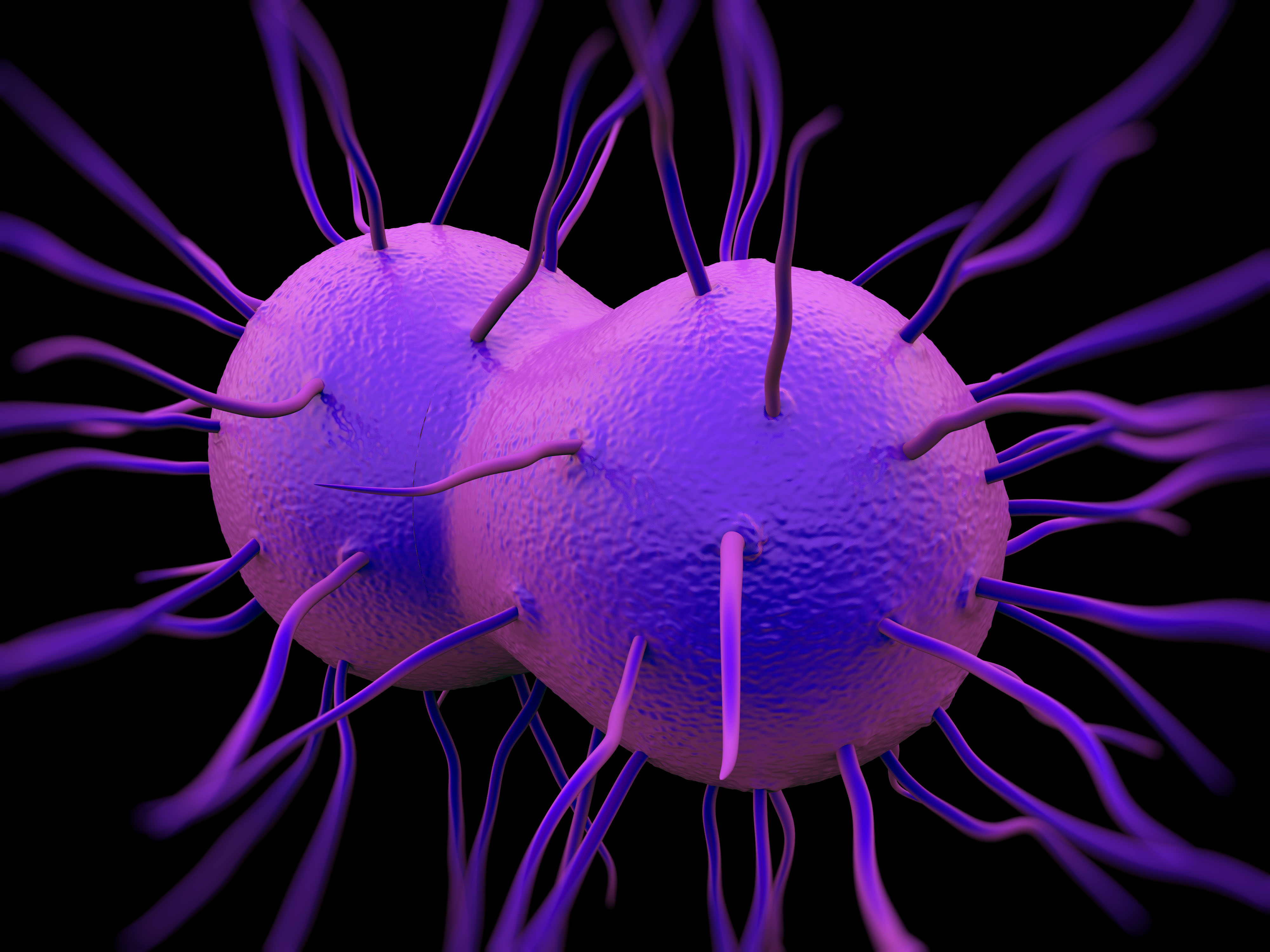
Colorized scanning electron micrograph of Neisseria gonorrhoeae bacteria, which causes gonorrhea. (NIAID via Flickr)
“We have great testing, [and the] medications are highly effective,” said Dr. Heidi Bauer, chief of the Sexually Transmitted Disease Control Branch of the California Department of Public Health. “This should not be an ongoing health problem. We should be able to do a much better job.”
The disease is continuing to spread in part because some people do not notify their partners so they can be treated, and local public health workers don’t always have the resources to track down and inform them, Bauer said.
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae, which can be transmitted through vaginal, anal or oral sex. Sometimes called “the clap,” the disease has afflicted humans at least since medieval times.
Gonorrhea can be cured with antibiotics, but if left untreated, it can cause infertility or inflammatory pelvic disease and increase the risk of contracting or transmitting HIV. Women often don’t know that they’re infected, because many don’t experience symptoms.
Typical symptoms in men include discharge from the penis or a burning sensation while urinating. But not all men experience these symptoms.
Rates of other sexually transmitted diseases are rising as well. The rate of syphilis has increased in California and nationally, though the actual number of cases is far smaller than for gonorrhea. Rates of chlamydia, which affects far more people than syphilis or gonorrhea, climbed about 7 percent between 2011 and 2014 among men and women of all ages.
However, the rate of AIDS among Californians age 13 years and older has declined.
In the universe of sexually transmitted diseases, gonorrhea traditionally hasn’t been as worrisome to public health officials as HIV/AIDS or syphilis, because its effects are not as severe and it can easily be treated.
New strains of antibiotic-resistant gonorrhea bacteria, however, have put epidemiologists around the world on alert.
Fortunately, new and aggressive treatment for gonorrhea, involving two types of antibiotics, appears to be keeping that strain at bay in California, Bauer said. Because many gonorrhea infections don’t cause symptoms, cases are increasingly being discovered through routine testing, Bauer said.
The increased rates are concentrated mostly among gay and bisexual men, and people age 15 to 24. There are regional differences, too. Rates are higher in California’s Central Valley and the Sacramento region than elsewhere in the state. Those differences might reflect variations in testing and access to care.
Clinicians now screen for asymptomatic infections in the mouth and anus, and some standard chlamydia tests also pick up gonorrhea infections. Use of PrEP – a medication regimen to prevent HIV infection – also has spurred more tests, because clinicians recommend that people using the regimen be tested for STDs every three months.
Bauer suggested that Californians newly insured under The Affordable Care Act and the state’s Medicaid expansion also may have increased access to testing.
But just because more people are insured doesn’t mean they have access to treatment, particularly in rural areas, said Claire Feldman, director of Statewide STD Prevention Programs for the California Family Health Council, which receives federal money for family planning and reproductive health services at clinics around the state.
Feldman noted that many county-run STD clinics have closed because primary care physicians increasingly include STD screening among their preventive health care services. And there’s too little funding for sexual health education, particularly among high risk groups, she said.
“There’s more screening, but that doesn’t mean that treatment and prevention are being provided to curb reinfection rates or the spread of these sexually transmitted diseases,” Feldman said. “It’s a very complex issue and there are no easy answers.”